No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
Antibacterial wash before surgery and in ICU
Numerous studies confirm that infections due to multi-drug-resistant organisms (MDRO) in the hospital are associated with high mortality,[1,2,3] lead to a two to three-fold longer period spent in hospital[4] and consequently involve higher directly attributable costs for diagnostics and therapy[5].
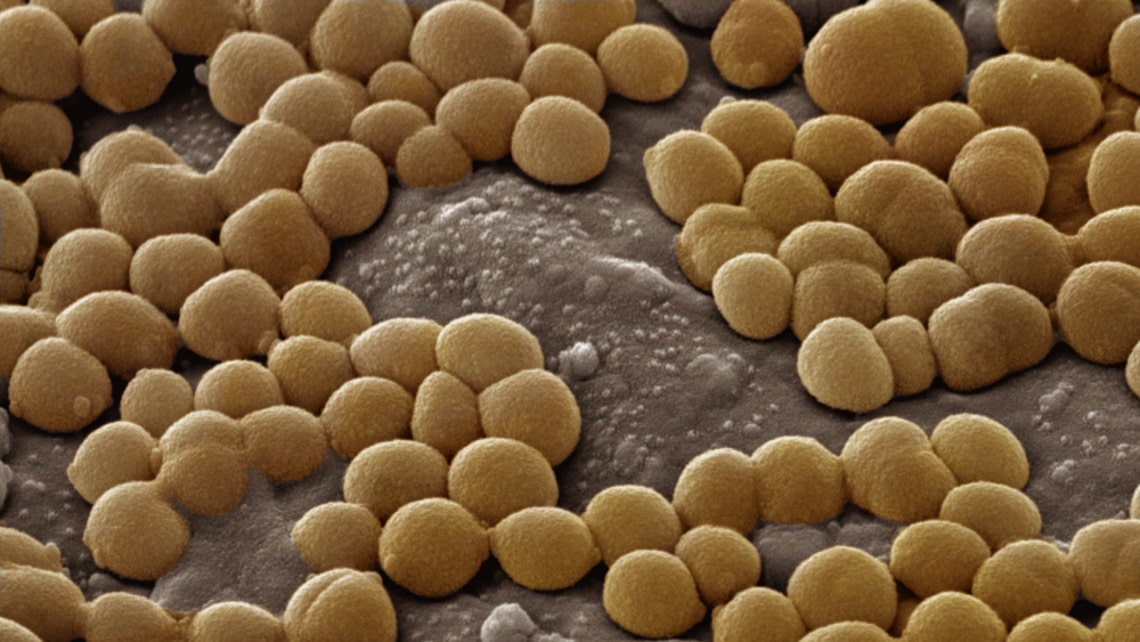
And in addition to multi-drug resistant organisms such as MRSA (Methicillin-resistant Staphylococcus aureus), other germs - both with low-grade as well as without any known antibiotic resistance - colonize the skin and mucous membranes of each prospective patient. These germs also can pose a serious and life-threatening infection risk to hospitalized patients[6,7].
Given these serious risks, could preventive whole-body decolonization with an antibacterial body wash be a magic bullet in the fight against infections and antibiotic-resistant pathogens inside the hospital?
Universal decolonization

We recommend that an antibacterial whole-body wash be performed on all patients as a universal decolonization before their elective hospitalization and surgery. This is intended to reduce the burden of colonization with microbials including MDRO[8].
The universal approach, by contrast to targeted decolonization, helps to avoid the problem of last-minute isolation of patients and potential postponement of surgeries[9],which often have involved a huge effort and drain on resources in patient management[4,5].
We know that there have been different approaches over time: First decolonization strategies focused on targeted decolonization for secondary prevention in those with recurrent episodes of Staphylococcus aureus disease. Then strategies changed to targeted decolonization for primary prevention by screening all patients for MRSA directly prior to surgery. Ultimately, universal decolonization for primary prevention has now moved strategically to the forefront[10].
Prehabilitation
Universal decolonization can be an effective measure within a bundled strategy against surgical site infections (SSI) and hospital-acquired infections in general[11].At the same time, it is intended to save costs compared to the targeted decolonization often practiced in hospitals[12].
Whole-body decolonization can be done by patients themselves as a preventive measure before elective surgery. But most of your patients probably aren’t aware that they can contribute to their own protection. Maybe they don’t know that they can prepare for surgery with an antibacterial whole-body decolonization intended to reduce infections.

As the surgeon, you can have an important role in preparing your patients for their elective hospitalization and engaging them for their own safety. You can empower them to be proactive in their healthcare which can lead to safer and more successful treatment outcomes for everyone involved. Recommend them an antibacterial whole-body wash with Prontoderm®, a leave-on product suitable for application at home and available as solution, foam, wipes, nasal gel, and mouth rinse solution.
Whole-body decolonization in hospital
Many people that have been admitted to the hospital are not able to take care of their hygiene themselves, as they are patients in the ICU or unable to move sufficiently even if they are on a regular ward. Many of them have a weakened immune system anyway and are therefore all the more dependent on protection against germs. Unfortunately, studies show that up to 30% of patients in intensive care can be affected by health care-associated infections[13].
Additionally, being in contact with many people in a hospital environment everyday requires prevention and protection, for all involved - including yourself.

With Prontoderm®, B. Braun is the reliable partner by your side offering a product concept that can help to reduce the risk of an infection. Prontoderm® products create a sustained antimicrobial barrier and inhibit the spread and transmission of microorganisms such as MDRO while setting new standards with the use of polyhexanide as a rinse-free and skin-compatible solution that does not lead to resistances[14].
Our solution

Prontoderm® is indicated for whole-body decolonization through physical cleansing. It is suitable for application in a medical environment or at home. Prontoderm® contains a synergistic mixture of surfactants and polyhexamethylene biguanide (preservative polyhexanide) in water. Surfactants and polyhexanide complement and support the physical cleansing.
Polyhexanide (PHMB):
A recent study found that polyhexanide in comparison to four other antimicrobials had the best ratio of bioactivity (antimicrobial activity) on the one hand to biocompatibility (skin tissue tolerance) on the other[14]. This means that polyhexanide acts powerfully against germs like Staphylococcus aureus and simultaneously protects the skin from damage[14].
Furthermore, it was shown that universal preoperative decolonization with polyhexanide effectively reduced Staphylococcus aureus-surgical site infections following elective joint arthroplasty[17].
Prontoderm®
Kindly check your inbox and confirm the email we've sent you.
*Methicillin-resistant Staphylococcus aureus
Your feedback matters! Participate in our customer survey to help us enhance our website, products and services. Thank you for your support!