No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
Decrease the potential risk of stoma leakage
Stoma complications can occur within one month after surgery but also at a later stage.[1] Some of the contributing factors may be the stoma placement, its characteristics, fistula formation or a high liquid output.[1] When any of these obstacles arise, effluents may irritate the peristomal skin and even seep under the stoma wafer.[2] As a result, the adhesion of the device can be compromised, and the surrounding area may also be irritated.[3]
If your patient suffers from stoma leakage, a convex stoma appliance may solve the issue. You can determine whether it is suitable by assessing the type of stoma and the patient’s abdominal contours.
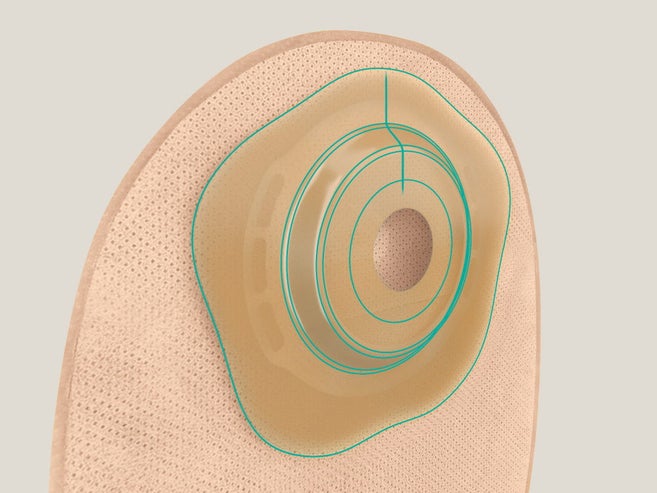
A convex ostomy bag system can possibly make the appliance adhere better to the surrounding skin to prevent stoma leakage, which is a frequent worry[4,5] for many ostomates. Convex ostomy bag systems are designed to[6,7,8,9]
The choice of soft convexity can bring additional advantages[8,9]

Depending on individual needs, you always have the option to choose between standard or soft convex stoma bags with deep or medium convexity. B. Braun has a whole range of convex options to suit your patients‘ needs. Find a good solution for each individual patient.
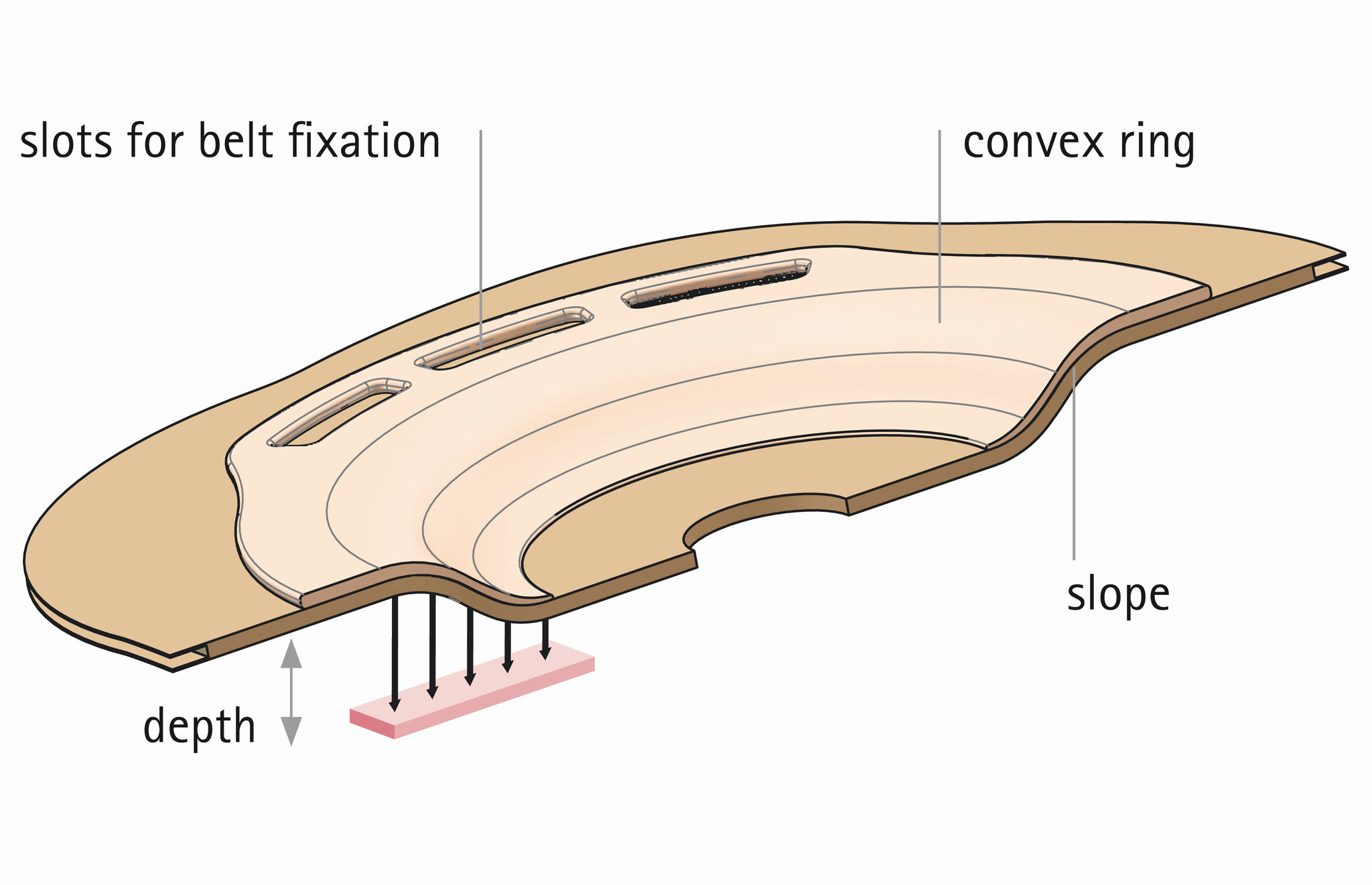
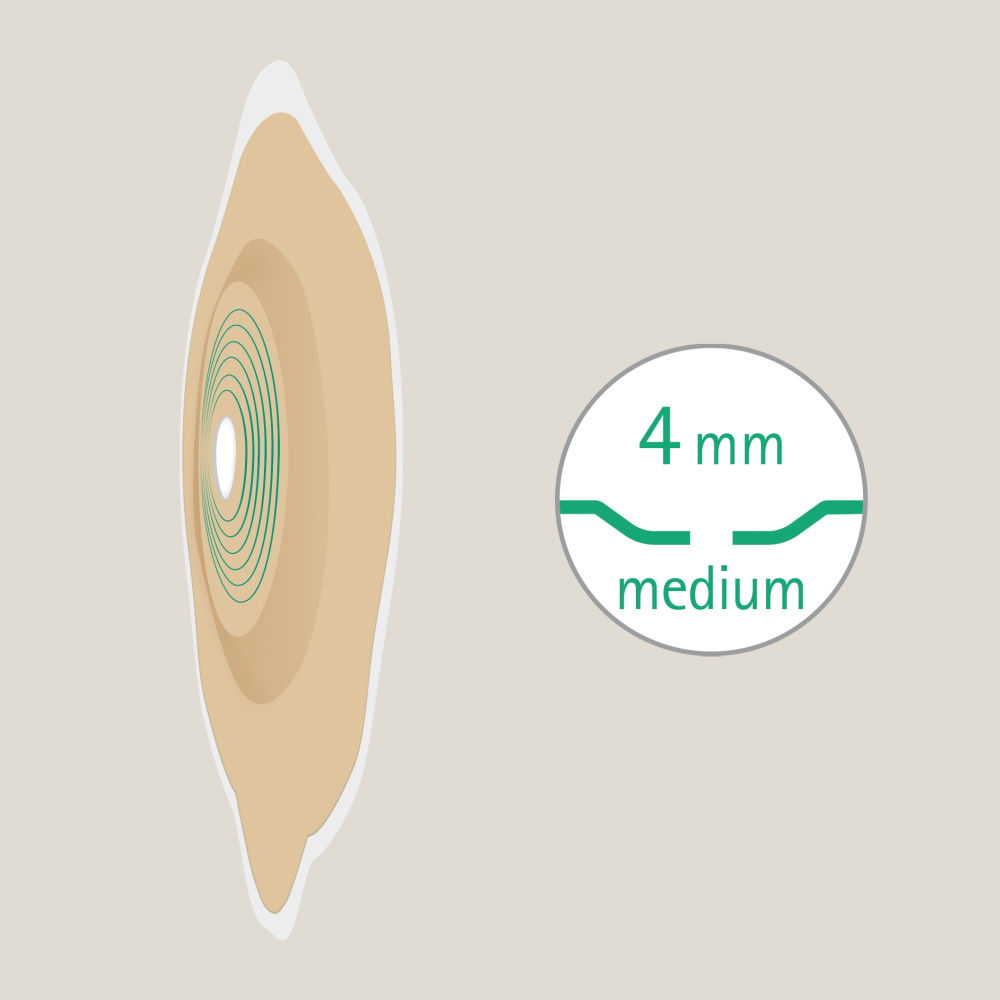
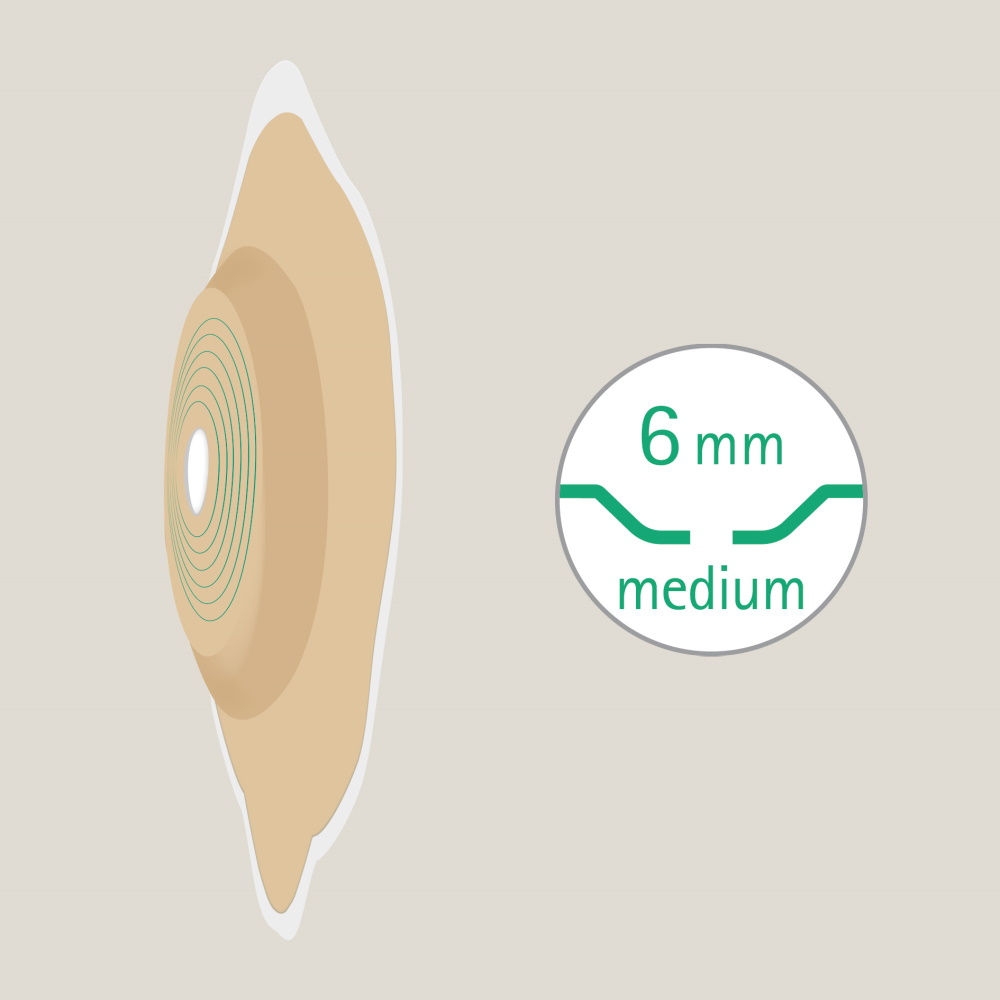
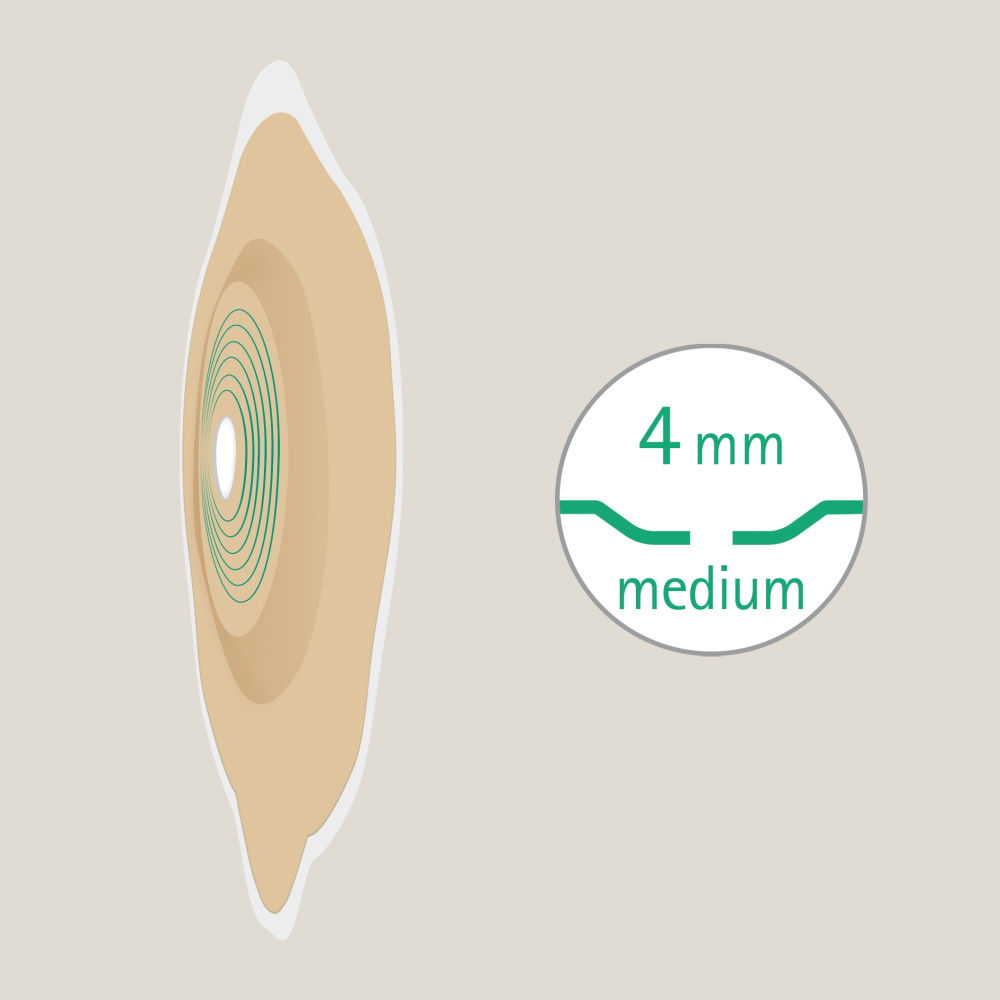
Gently sloping convexity is a feature of all 4 to 6 mm products. It was developed to provide better pressure distribution and to apply sufficient pressure around the stoma to shape and form the patient’s peristomal contours.
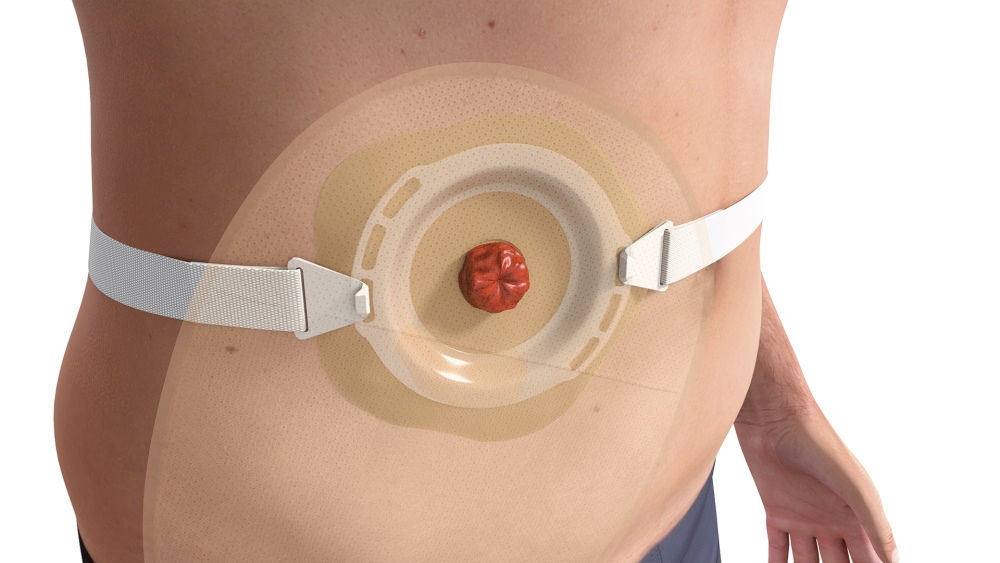
To create a higher sense of security, many users recommend the use of a stoma belt to intensify the effect of convexity. Three different attachment positions* allow the belt to match the preferred position of the bag on the abdomen.

Discover the latest generation of soft convex stoma bags: Flexima® Active O' convex

“I’ve seen some great results using Flexima Active O ´convex with patients with "uneven" peristomal surroundings. The soft convex is "soft enough" and has the "needed pressure" for this kind of skin. You know the bellies and stomas are usually not ideal, as literature shows. But our patients need the help to live normally. And one solution for me now is Flexima Active O´ convex.”

“I love Softima Active Convex Uro. It gives me the option to use a soft convex appliance (and belt) on some friable post-op stomas where I might be hesitant to use a "normal" convex one. I’ve seen some great results using this with patients recently where I was worried about pressure around the mucocutaneuos junction. I find the convexity is soft yet stable and that’s what makes the difference!”
The flexible convex wafer allows flat stomas to protrude and to seal stomas in folds. It can even fill in small hollows while simultaneously limiting the peristomal pressure. Moreover, the flexible ring can create a seal around the stoma.
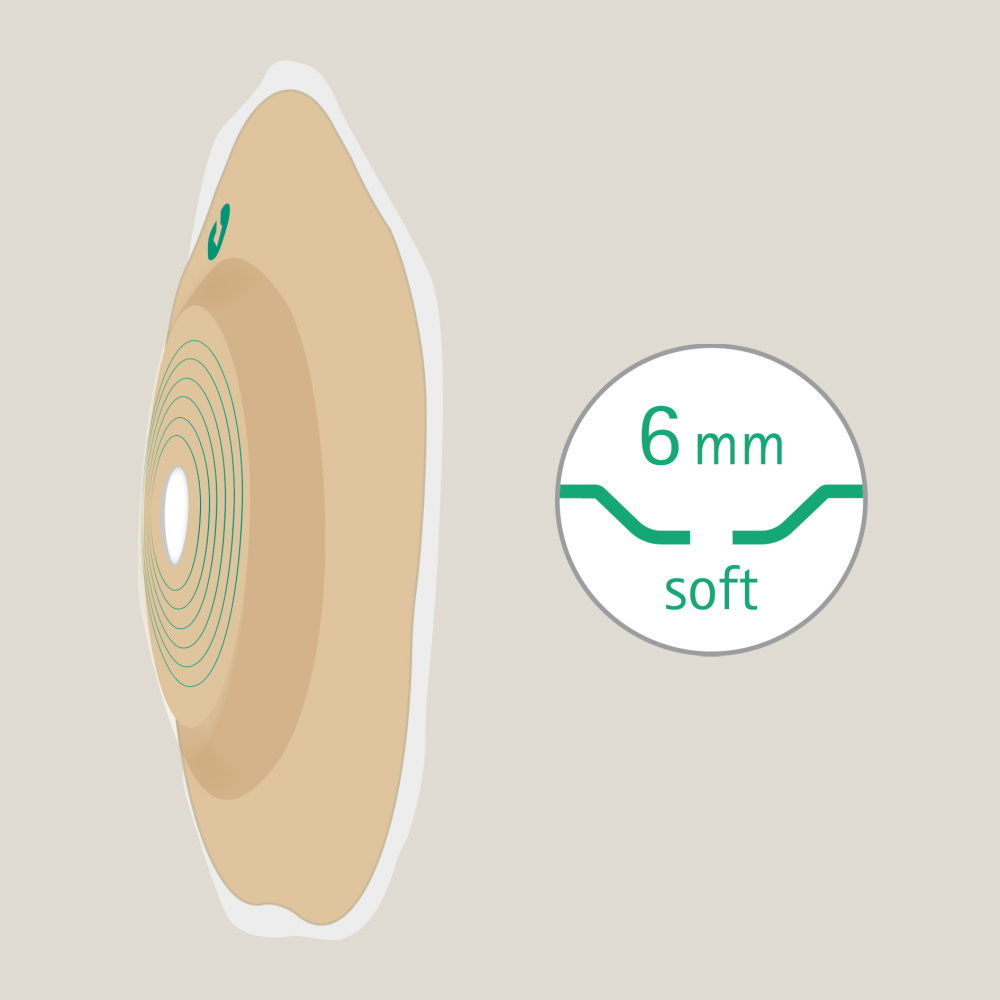
Moderate convexity of 4 mm can help make the stoma protrude.
Moderate convexity of 6 mm can help fill in medium to deep hollows and the folds in the skin.
Moderate convexity of 4 mm can help make the stoma protrude.
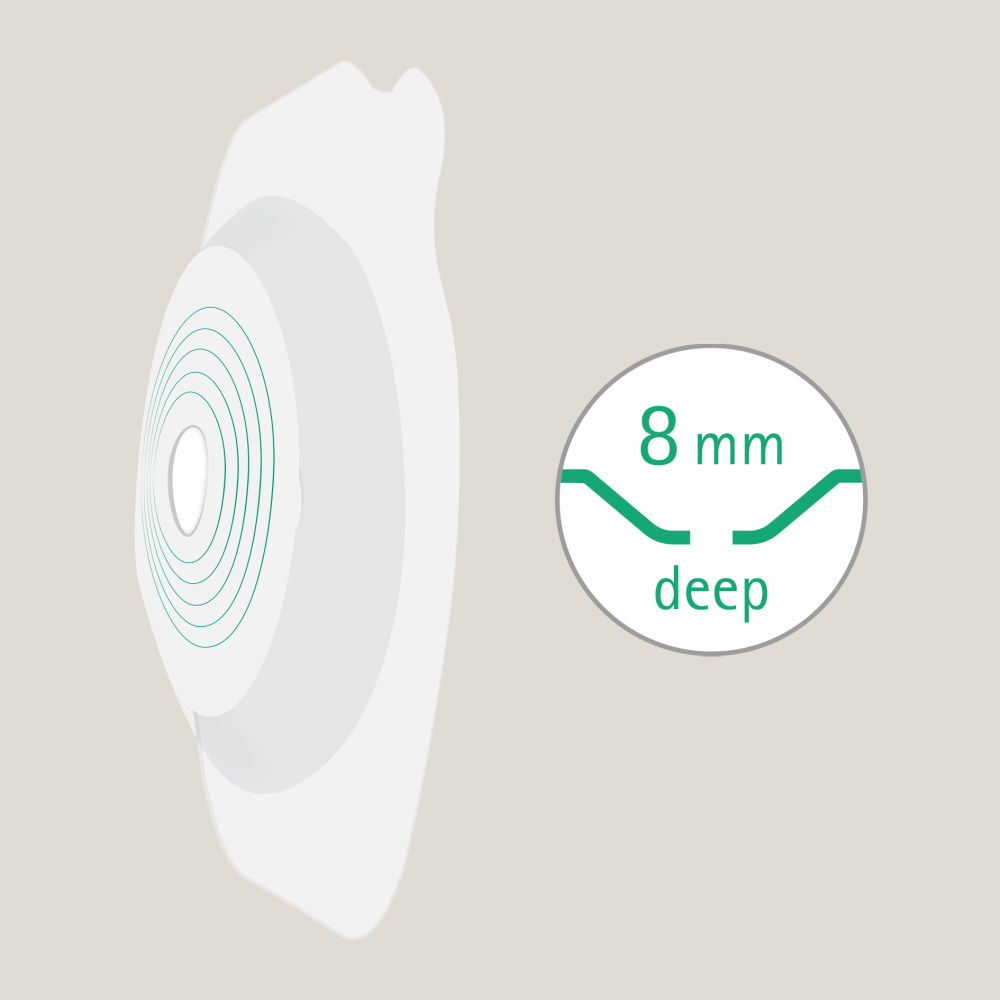
Deep convexity can help fill in deep hollows and skin folds.
Just as every person is unique, so is every stoma. That’s why B. Braun offers a diverse range of ostomy care accessories to personalize the care of your patient.
Discover our products
* except for Proxima® 2+, which has one hooking position for the belt
Your feedback matters! Participate in our customer survey to help us enhance our website, products and services. Thank you for your support!