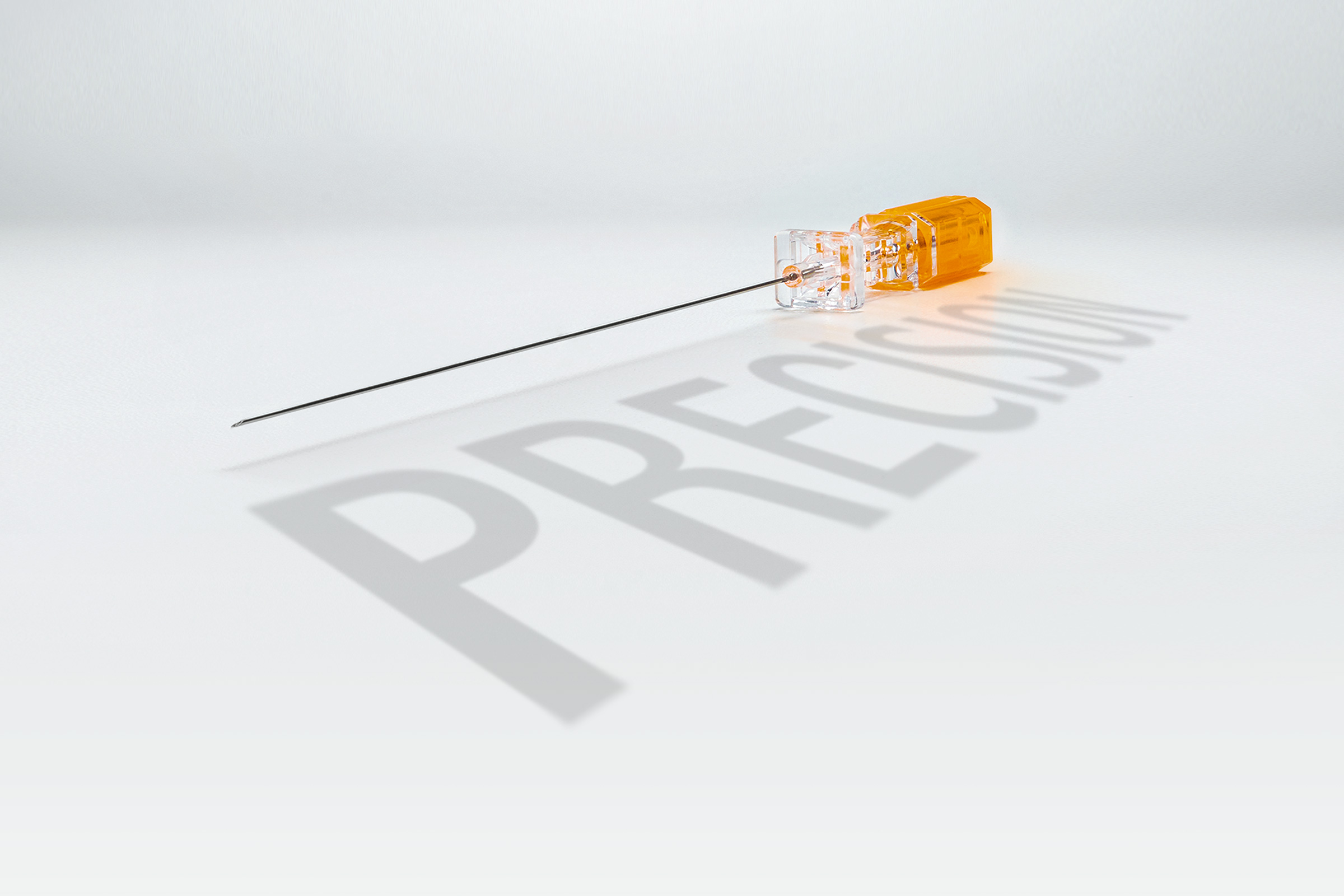
Pencan® - atraumatic needle:
Advanced technology for decreasing incidence of post lumbar puncture headaches.
You have successfully logged out.
Not registered yet?
Atraumatic Needles for Spinal Anesthesia
Spinal anesthesia is widely used, yet 5–8% of attempts fail1, often requiring conversion to general anesthesia—causing delays, discomfort, and higher complication risks like post-dural puncture headache (PDPH).
Discover how needle design impacts spinal anesthesia success.2
Learn why atraumatic Pencan® needles reduce PDPH risk and improve patient safety.
Spinal Anesthesia
up to
0%
Clinical guidelines and systematic reviews consistently endorse atraumatic, pencil-point needles as the superior option for spinal anesthesia and lumbar puncture.3 The atraumatic, ogival tip of Pencan® separates dural fibers rather than cutting them, reducing Cerebrospinal Fluid (CSF) leakage and tissue damage.4
Compared to traditional cutting-tip designs, Pencan® significantly lowers the risk of post-dural puncture headache, enhances patient safety, and improves overall procedural outcomes.5
Clinical data show that the use of Pencan® significantly reduces the incidence of post-lumbar puncture headaches—from 7.6% with conventional needles to just 2.3%. In addition, the need for an epidural blood patch is markedly lower, decreasing from 1.8% to only 0.5%.
Advanced technology for decreasing incidence of post lumbar puncture headaches.

One risk factor for post lumbar puncture headaches is the use of Quincke needle.
It is well established that atraumatic needle designs help reduce the risk of PDPH. However, atraumatic needles vary significantly between manufacturers in terms of tip geometry, orifice length, and eyelet positioning6. These differences can impact performance, safety, and user experience.7 Choosing the right atraumatic needle is essential—not just any atraumatic needle will do.

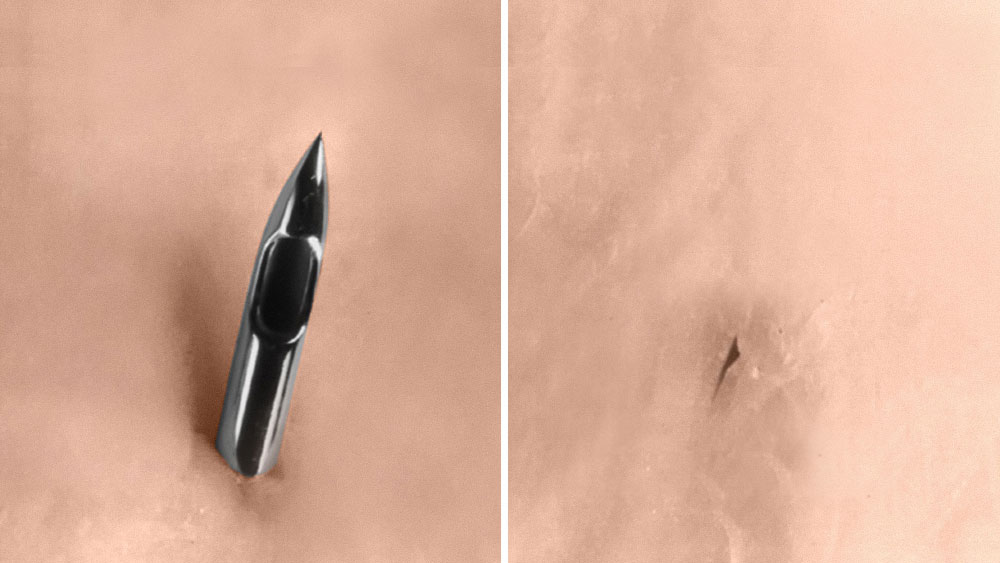
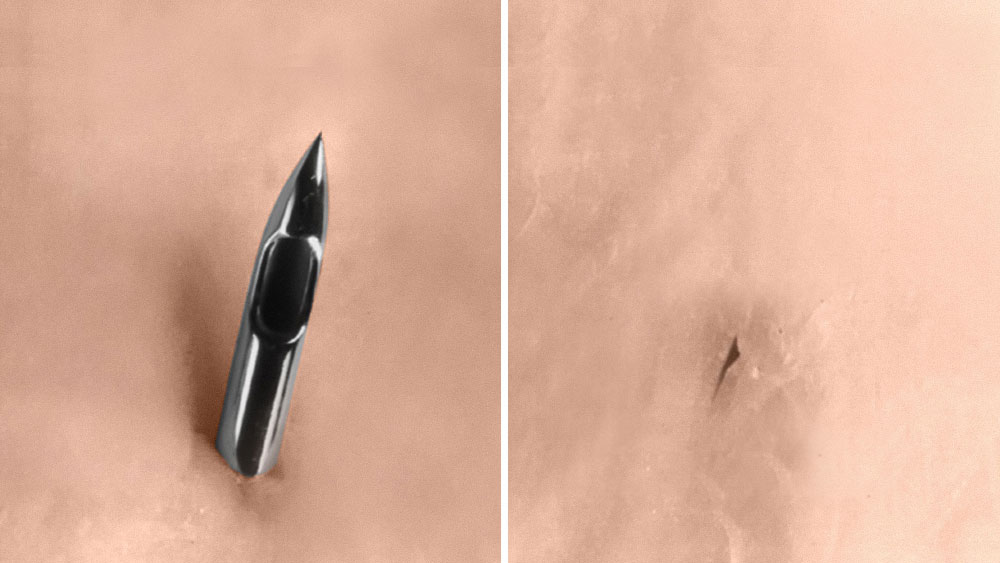
To deliver anesthetic effectively, the spinal needle must pass through several anatomical layers: skin, subcutaneous tissue, ligaments, and the dura mater. Success is confirmed by the appearance of CSF in the needle hub. However, needle design affects how reliably and safely this confirmation occurs. Poorly designed needles can result in partial placement, where the orifice lies between the subarachnoid and epidural spaces. This can lead to incomplete drug delivery and failed anesthesia, despite apparent CSF flashback 8 (Fig 1)
A shorter tip-to-back-of-eyelet distance helps minimize the insertion depth of the needle tip into the subarachnoid space, reducing the risk of nerve contact and ultimately lowering the chance of paresthesia.9 ( Fig.2) It also enables faster CSF return for better control during placement.
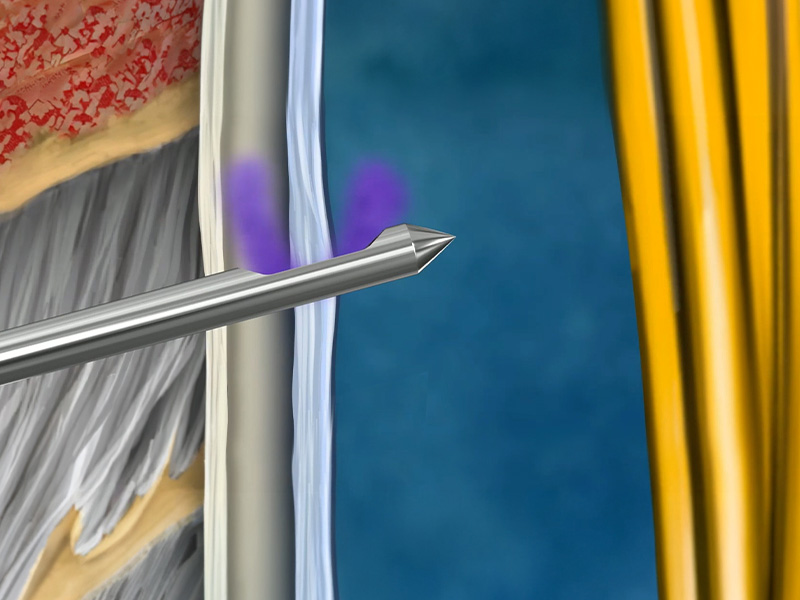
Fig.1
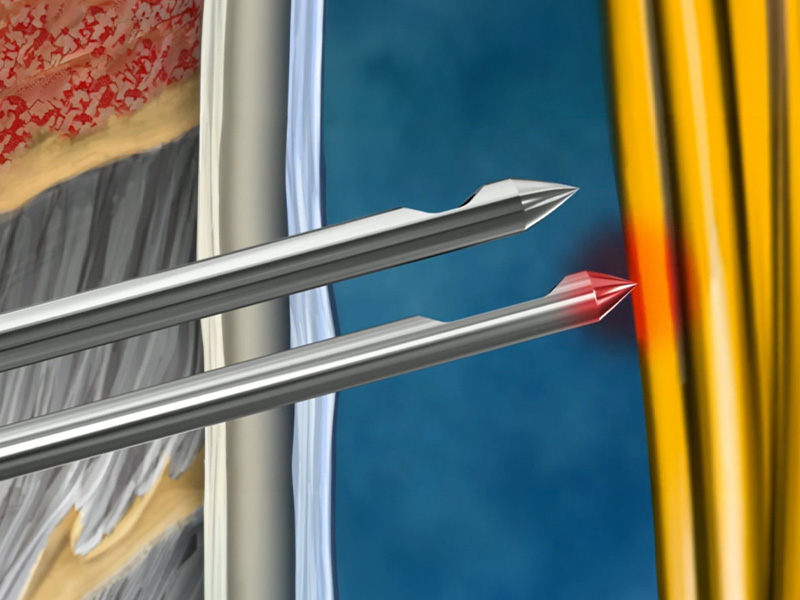
Fig.2
Support full intrathecal delivery and help to reduce the likelihood of partial or incomplete anesthesia.
Optimized eyelet positioning designed to enable faster CSF flashback, aiding correct and quick placement - reducing the need for multiple attempts.
Provides a clear “dural pop” for tactile feedback, helps minimize nerve contact, and promotes a clean dural tear—associated with lower PDPH rates.
Designed to reduce the risk of cauda equina contact, especially important in pediatric patients.
WHO recommendations
Intrapartum care for a positive childbirth experience - WHO recommendations: intrapartum care for a positive childbirth experience
link
WFSA Labour Analgesia Declaration
Labour Analgesia Declaration – WFSA
link
ASA Practice Guidelines for Obstetric Anesthesia
An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology Anesthesiology
link
ASA Statement on Neuraxial Analgesia or Anesthesia in Obstetrics
Standards and Practice Parameters Statement on Neuraxial Anesthesia in Obstetrics
link
A responsible contact person will get in touch with you as soon as possible.
1. Kinsella, S.M. (2008). A prospective audit of regional anaesthesia failure in 5080 Caesarean sections. Anaesthesia, 63(8), 822–832. doi: 10.1111/j.1365-2044.2008.05499.x.
2. Batova, R., & Georgiev, S. (2019). Impact of spinal needle design and approach on postdural puncture headache and spinal anesthesia failure in obstetrics. Anaesthesiology Intensive Therapy, 51(2), 77–82. doi: 10.5114/ait.2019.86166.
3. Nath, S., Koziarz, A., Badhiwala, J. H., et al. (2018). Atraumatic versus conventional lumbar puncture needles: A systematic review and meta-analysis. The Lancet, 391(10126), 1197–1204. https://doi.org/10.1016/S0140-6736(18)30493-6
4. Xu H, Liu Y, Song W, Kan S, Liu F, Zhang D, Ning G, Feng S. Comparison of cutting and pencil-point spinal needle in spinal anesthesia regarding postdural puncture headache: A meta-analysis. Medicine (Baltimore). 2017 Apr;96(14):e6527. doi: 10.1097/MD.0000000000006527. PMID: 28383416; PMCID: PMC5411200.
5. Reina, M. A., Puigdellívol-Sánchez, A., Gatt, S. P., De Andrés, J. A., Prats-Galino, A., & van Zundert, A. (2017). Electron microscopy of dural and arachnoid disruptions after subarachnoid block. Regional Anesthesia and Pain Medicine, 42(6), 709–718. https://doi.org/10.1097/AAP.0000000000000667
6. B. Braun technical data report, 2025
7. Reina, M. A., López, A., De Andrés, J. A., Prats-Galino, A., & van Zundert, A. (2007). Variability in the design of spinal needles: Implications for clinical practice. Regional Anesthesia and Pain Medicine, 32(4), 346–353. https://doi.org/10.1016/j.rapm.2007.02.006
8. Rae, J. D., & Fettes, P. D. W. (2023). Mechanisms and management of failed spinal anesthesia. NYSORA – The New York School of Regional Anesthesia. Retrieved from https://www.nysora.com/topics/complications/mechanisms-management-failed-spinal-anesthesia/
9. Reina MA, De Andres JA, Hernández JM, Arriazu Navarro R, Pastor J, Prats-Galino A. Looking for the development of paresthesias in the subarachnoid and epidural anesthesia: A clinical and anatomical analysis. Reg Anesth Pain Med. 2011;36(Suppl):E17–E22. doi:10.1097/AAP.0b013e3182030648.
Your feedback matters! Participate in our customer survey to help us enhance our website, products and services. Thank you for your support!