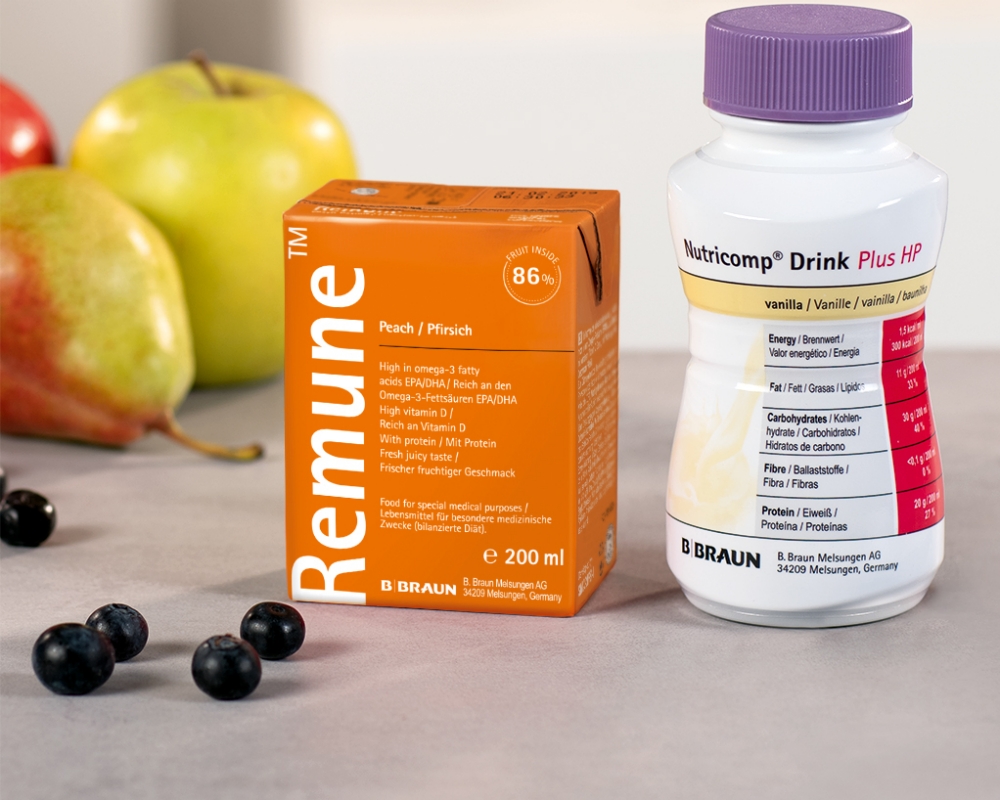
Nutricomp® – Wide variety of taste
The fully balanced Nutricomp® Drink Food for Special Medical Purposes (FSMP) range has nutritionally complete milk-based, gluten free formulas containing essential nutrients, vitamins and minerals.
They can be used as supplementary or complete nutrition with the following benefits:
- Ready to drink, also suitable for tube feeding as the bottle connects to a wide neck adaptor for any given set
- The bottle design provides a handy grip and easy opening due to a foil
- Best served chilled or shortly heated in the microwave in a bowl or cup (max. 60 °C) (especially suitable for Nutricomp® Soup)
Why Nutricomp® in oncology?
Cancer is one of the major healthcare burdens worldwide and one of the leading causes of death in many countries. Progress in anticancer therapies has improved cancer survival rates.1,2 Malnutrition is a common problem in cancer patients that has been recognized as an important component of adverse outcomes, including increased morbidity and mortality and decreased quality of life.3
Cancer patients commonly suffer from weight loss, which serves as an indicator of poor prognosis in cancer patients.4 Cancer cachexia is observed in approximately 50-80% of advanced cancer patients.5
Nutrition plays an important role in many aspects of cancer development and is an important supportive therapy throughout the whole pathway of cancer treatment. Adequate nutrition support can help cancer patients maintain weight and lean body composition, may offer better recovery from nutrition impact symptoms and may improve quality of life.6,7,8
General literature
1 Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2) [published correction appears in Lancet. 2015 Mar 14;385(9972):946]. Lancet. 2015;385(9972):977-1010.
2 Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271-289.
3 Santarpia L, Contaldo F, Pasasini F. Nutritional sccreening and early treatment of malnutrition in cancer patients. J Cachexia Sarcopenia Muscle. 2011 Mar, 2(1):27-35.
4 Hébuterne X, Lemarié E, Michallet M, de Montreuil CB, Schneider SM, Goldwasser F. Prevalence of malnutrition and current use of nutrition support in patients with cancer. JPEN J Parenter Enteral Nutr. 2014;38(2):196-204.
5 von Haehling S, Anker MS, Anker SD. Prevalence and clinical impact of cachexia in chronic illness in Europe, USA, and Japan: facts and numbers update 2016. J Cachexia Sarcopenia Muscle. 2016;7(5):507-509.
6 Yan X, Zhou FX, Lan T, et al. Optimal postoperative nutrition support for patients with gastrointestinal malignancy: A systematic review and meta-analysis. Clin Nutr. 2017;36(3):710-721.
7 Kreitler S, Barak F, Danieli-Siegelman N, Ostrowsky A. Nutrition and quality of life in advanced cancer patients. Supportive care of cancer. 2012; 20 (Supl1): 132-133.
8 Isenring EA, Capra S, Bauer JD. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer. 2004;91(3):447-452.