No content results match your keyword.
Content
You have successfully logged out.
Not registered yet?
Difficult IV access
Establishing functional peripheral intravenous access is a routine in both the emergency and inpatient setting. While the traditional method of vein palpation for cannulation is successful in the majority of patients, patients with difficult intravenous access present a daily challenge to hospital staff.1

Difficult intravenous access (DIVA) is generally understood as arising when two or more punctures are performed without success, or when puncture support methods are required, or when the impossibility of obtaining peripheral access means that a central venous catheter (CVC) must be inserted.2,3,4
In fact, more than 30% of adults and up to 50% of children who require a PIVC (peripheral intravenous catheter) are reported to have challenging venous access.2
Catheter-related complications further complicate the situation. Up to 90% of short peripheral IV catheters fail before therapy completion.6
50% fail within 24 hours.7
The group of potential DIVA patients is large:
Pediatric patients, overweight and obese patients, elderly and chronically ill patients, and acute patients. They all search for deep veins.2,3
In pediatric patients, the first stick success rate is less than 35% due to thicker tissue layers.8


In overweight and obese patients, multiple attempts are usually necessary due to the thicker subcutaneous adipose tissue layer, which in turn is associated with two risks.8,9 First, the puncture error rate increases, and second, the risk of infiltration is increased. According to the WHO, obesity has nearly tripled worldwide since 1975 and is expected to increase further in Europe.10,11
Elderly and chronically ill patients, such as those suffering from diabetes, have weaker vascular systems. In the U.S., 14.5% of people are over 65 years old, and 422 million suffer from diabetes.13


Injuries in emergency and acute care patients, such as skin burns, hematomas, or dehydration, result in difficult intravenous access in approximately 11% of patients in the emergency room.14
Difficult IV access is usually associated with repeated insertion attempts and catheter-related complications. These are not only time-consuming and material-intensive, but also lead to an increased stress level among the nursing staff and the patient, combined with an increased perception of pain.9
In the emergency department in particular, the problem of DIVA has been found to negatively impact both patient safety and satisfaction. For example, multiple failed attempts to insert vascular access often result in patients becoming increasingly agitated, exhibiting "needle phobia", and losing trust in healthcare professionals. Patients may develop pain or bruising at the insertion sites, putting them at higher risk for skin injury and infection. Delayed access can further increase the time needed for necessary diagnoses or treatments such as fluid resuscitation and administration of medications or pain medications.2 Complementing this, multiple punctures may be associated with progressive deterioration of the vascular tree, termed "vascular exhaustion", which further complicates vascular access during successive contacts with the patient.15

Once cannulated, survival of IV catheters is problematic.
Nearly
0%
of PIVC are terminated early due to complications such as dislodgement, infiltration or extravasation.6
Dislodgement is when the catheter loses access to the patient's vasculature and causes a forced, premature interruption of infusion therapy. Infiltration or extravasation, on the other hand, occurs when punctures do not properly target the vascular access and cause the infused solution to flow into the tissue surrounding the vascular access. This complication is particularly relevant when infusing highly irritating (e.g., vesicant) substances.6

In addition to nerves and time, repeated insertion attempts cost material above all. For example, the average cost of replacing PIVCs per sequence of IV treatment is USD 51.92.17 Repeated unsuccessful insertion of a PIVC sometimes leads to switching to more expensive and complex solutions and using central venous catheters (CVC) or peripherally inserted central catheters (PICC – peripherally inserted central venous catheter).
Both alternatives require a longer insertion process and are associated with higher material costs. However, in many cases, CVCs are inserted unnecessarily. Although patients are eligible for a peripheral IV catheter, CVC or PICC are used because of difficult IV access rather than dwell time or infusion solution.18
0min
per insertion3
The average time required for a peripheral intravenous cannulation is reported to be 2.5 to 13 minutes.
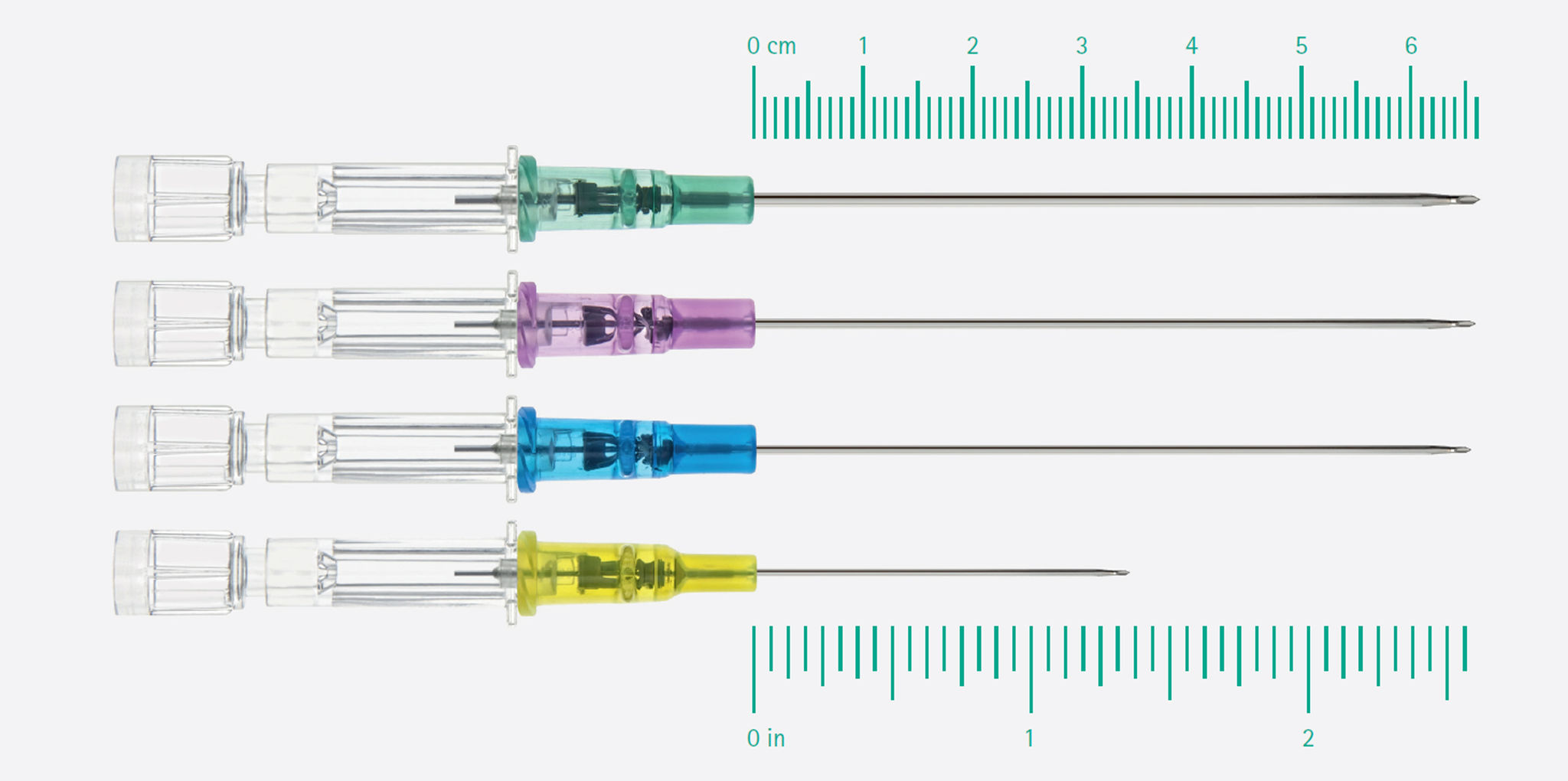
To treat patients with difficult intravenous access in a time-, nerve-, and material conserving manner, the use of longer PIVC and ultrasound-assisted catheter insertion is recommended.
Long PIVCs increase catheter survival time. A longer part of the capillary stays in the vein and helps to prevent catheter dislodgements and infiltrations.16,18,20,21,22
According to Bahl et al 2019, the optimal length of the catheter in the vein is at least 2.75cm.
Furthermore, ultrasound-guided venipuncture supports first-stick success.22,23,24
Median dwell time
0
days16
First stick success rate
0%
Under ultrasound guidance19
Therapy completion
0%
Remained complication free for the required duration of therapy19
“Long catheter ultrasound-guided procedure is associated with a lower risk of catheter failure compared with short catheter ultrasound-guided procedure.”20

1. Bahl A, Hang B, Brackney A, Joseph S, Karabon P, Mohammad A, ... & Shotkin P. Standard long IV catheters versus extended dwell catheters: A randomized comparison of ultrasound-guided catheter survival. The American journal of emergency medicine. 2019;37(4);715-721.
2.Whalen M, Maliszewski B, Baptiste DL. Establishing a Dedicated Difficult
Vascular Access Team in the Emergency Department: A Needs Assessment. J InfusNurs. 2017 May/Jun;40(3):149-154.
3. Crowley M, Brim C, Proehl J, Barnason S, Leviner S, Lindauer C, Naccarato M,Storer A, Williams J, Papa A. Emergency nursing resource: difficult intravenous access. Journal of emergency nursing. 2012 Jul 1;38(4):335-43.
4. Rodríguez-Calero MA, Blanco-Mavillard I, Morales-Asencio JM, FernándezFernández I, Castro-Sánchez E, de Pedro-Gómez JE. Defining risk factors associated with difficult peripheral venous Cannulation: A systematic review and meta-analysis. Heart & Lung. 2020 May 1;49(3):273-86.
5. Bertoglio S, van Boxtel T, Goossens GA, Dougherty L, Furtwangler R, Lennan E, Pittiruti M, Sjovall K, Stas M. Improving outcomes of short peripheral vascular access in oncology and chemotherapy administration. The Journal of Vascular Access. 2017 Mar;18(2):89-96.
6. Helm RE, Klausner JD, Klemperer JD, Flint LM, Huang E. Accepted but unacceptable: peripheral IV catheter failure. Journal of Infusion Nursing. 2015 May 1;38(3):189-203
7. Steere L, Ficara C, Davis M, Moureau N. Reaching one peripheral intravenous catheter (PIVC) per patient visit with lean multimodal strategy: the PIV5Rights™ bundle. Journal of the Association for Vascular Access. 2019;24(3):31-43.
8. Nafiu OO, Burke C, Cowan A, Tutuo N, Maclean S, Tremper KK. Comparing peripheral venous access between obese and normal weight children. Paediatr Anaesth. 2010 Feb;20(2):172-6
9. Fields JM, Piela NE, Ku BS. Association between multiple IV attempts and perceived pain levels in the emergency department. J Vasc Access. 2014;15:514–8
10. WHO Obesity and overweight https://www.who.int/news-room/fact sheets/detail/obesity-and-overweight
11. Pineda E, Sanchez-Romero LM, Brown M, Jaccard A, Jewell J, Galea G, Webber L, Breda J. Forecasting Future Trends in Obesity across Europe: The Value of Improving Surveillance. Obes Facts. 2018;11(5):360-71.
12. (Department of Health AU, PIVC Guideline) https://www.health.qld.goc.au/_data/assets/pdf_file/0025/444490/icare-pivc-guideline-pdf
13. Wengström Y, Margulies A; European Oncology Nursing Society Task Force. European Oncology Nursing Society extravasation guidelines. Eur J Oncol Nurs. 2008 Sep;12(4):357-61
14. Dychter Samuel S. MD, Gold David A PhD, Carson Deborah RN, Haller, Michael PhD. Intravenous Therapy: A Review of Complications and Economic Considerations of Peripheral Access. Journal of Infusion Nursing. 2012 Mar;35(2);84-91.
15. Moraza-Dulanto MI, Garate-Echenique L, Miranda-Serrano E, ArmenterosYeguas V, Tomás-López MA, Benítez-Delgado B. Inserción eco-guiada de catéteres centrales de inserción periférica (PICC) en pacientes oncológicos y hematológicos: éxito en la inserción, supervivencia y complicaciones. Enferm Clin. 2012;22(3);135–143
16. Bahl, A., Hijazi, M., Chen, N.W., Clavette-Lachapelle, L. and Price, J., 2019. Ultra Long versus Standard Long Peripheral Intravenous Catheters: A Randomized Controlled Trial of Ultrasound-Guided Catheter Survival. Available at SSRN 3401988
17. Marsh N, Webster J, Larson E, Cooke M, Mihala G, Rickard CM. Observational Study of Peripheral Intravenous Catheter Outcomes in Adult Hospitalized Patients: A Multivariable Analysis of Peripheral Intravenous Catheter Failure. J Hosp Med. 2018 Feb 1;13(2):83-89
18. Paladini A, Chiaretti A, Sellasie KW, Pittiruti M, Vento G. Ultrasound-guided placement of long peripheral cannulas in children over the age of 10 years admitted to the emergency department: a pilot study. BMJ Paediatr Open. 2018 Mar 28;2(1):e000244
19. Godfrey J, Gallipoli L. Introducing a long peripheral catheter to support improved outcomes for difficult access (DIVA) patients. 2022 Oct. World Congress of Vascular Access.
20. Elia, F., Ferrari, G., Molino, P., Converso, M., De Filippi, G., Milan, A. and Aprà, F., 2012. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. The American journal of emergency medicine, 30(5), pp.712-716.
21. Meyer P, Cronier P, Rousseau H, Vicaut E, Choukroun G, Chergui K, Chevrel G, Maury E. Difficult peripheral venous access: clinical evaluation of a catheter inserted with the Seldinger method under ultrasound guidance. Journal of critical care. 2014 Oct 1;29(5):823-7.
22. Scoppettuolo G, Pittiruti M, Pitoni S, Dolcetti L, Emoli A, Mitidieri A, Migliorini I, Annetta MG. Ultrasound-guided “short” midline catheters for difficult venous access in the emergency department: a retrospective analysis. International journal of emergency medicine. 2016 Dec;9(1):1-7.
23. Vinograd, A.M., Chen, A.E., Woodford, A.L., Fesnak, S., Gaines, S., Elci, O.U. and Zorc, J.J., 2019. Ultrasonographic Guidance to Improve First-Attempt Success in Children With Predicted Difficult Intravenous Access in the Emergency Department: A Randomized Controlled Trial. Annals of emergency medicine.
24. Stolz LA, Stolz U, Howe C, Farrell IJ, Adhikari S. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. The journal of vascular access. 2015 Jul;16(4):321-6.
Your feedback matters! Participate in our customer survey to help us enhance our website, products and services. Thank you for your support!